Navigating the Complex World of Workers’ Compensation Providers: A Comprehensive Guide
Workers’ compensation insurance is a critical safety net for employees injured on the job. Understanding the providers of this insurance, however, can be a daunting task. This guide delves into the various types of workers’ compensation providers, their roles, and how to choose the right one for your needs, whether you’re an employer, employee, or healthcare provider.
Types of Workers’ Compensation Providers
-
Insurance Companies:
These are the most common type of workers’ compensation provider. They offer policies to employers, covering medical expenses and lost wages for employees injured at work. Different insurance companies have varying levels of service, claim processing speeds, and cost structures. Choosing the right insurance company often involves comparing quotes, reading reviews, and understanding the specific coverage offered.
-
Self-Insurance:
Larger companies with substantial financial resources may opt for self-insurance. This means they assume the financial risk of workers’ compensation claims themselves, often setting up a dedicated fund to manage these costs. Self-insurance requires significant financial reserves and robust internal risk management processes. It often involves hiring specialized staff to manage claims and ensure compliance with regulations.
-
State Funds:
Some states operate their own workers’ compensation insurance funds. These funds provide coverage to employers who may have difficulty obtaining insurance through private insurers, often due to high-risk industries or poor safety records. State funds generally operate under stricter regulations and may offer more standardized benefits compared to private insurers. They also often have specific requirements and processes for claims handling.
-
Third-Party Administrators (TPAs):
TPAs are not insurers themselves but rather manage workers’ compensation claims on behalf of insurance companies or self-insured employers. They handle tasks such as processing claims, managing medical bills, and communicating with injured workers and healthcare providers. TPAs can bring expertise in claims management and potentially streamline the claims process for their clients.
-
Managed Care Organizations (MCOs):
MCOs are healthcare providers that manage the medical care aspect of workers’ compensation claims. They coordinate care, negotiate rates with healthcare providers, and monitor treatment to ensure cost-effectiveness and appropriate medical care. MCOs are frequently used by insurers and self-insured employers to control costs and ensure quality medical services for injured workers.
Choosing the Right Workers’ Compensation Provider
The best workers’ compensation provider depends on your specific circumstances and priorities. Several factors should be considered:
-
Cost:
Premiums vary widely depending on the provider, industry, and employer’s safety record. Balancing cost with the level of service and coverage is crucial. A cheaper provider might offer limited benefits or slower claim processing.
-
Claims Processing Speed and Efficiency:
A provider with a reputation for efficiently and fairly handling claims can significantly reduce stress for both employers and employees. Researching claim processing times and customer reviews is essential.
-
Customer Service:
Having easy access to a responsive and helpful customer service team can make a huge difference during a stressful time. A provider’s communication style and responsiveness should be considered.
-
Network of Healthcare Providers:
Access to a wide network of qualified healthcare providers can ensure employees receive timely and appropriate medical care. This is particularly important for employees requiring specialized treatment.
-
Financial Stability:
Choosing a financially stable provider ensures that benefits will be paid even in the event of unexpected claims or economic downturns. Checking the provider’s financial ratings can provide valuable insights.
-
Compliance with Regulations:
All workers’ compensation providers must comply with state and federal regulations. Choosing a provider with a strong track record of compliance minimizes legal risks for employers.
-
Level of Coverage:
Policies vary in the types and extent of coverage provided. Understanding the specific benefits covered (medical care, lost wages, rehabilitation, etc.) is crucial.
Understanding the Workers’ Compensation Claims Process
Regardless of the provider, the workers’ compensation claims process generally involves several steps:
-
Reporting the Injury:
Employees must promptly report workplace injuries to their employer. The reporting procedure will vary based on the employer’s policies and the severity of the injury.
-
Filing a Claim:
The employer typically files a claim with the workers’ compensation provider. This involves providing information about the injury, the employee’s medical treatment, and lost wages.
-
Medical Treatment:
The provider typically designates healthcare providers who will treat the injured employee. Access to a wide network of healthcare providers is crucial for timely and appropriate treatment.
-
Claim Review and Approval:
The provider reviews the claim and determines the validity of the injury and the extent of benefits payable. This process can involve medical evaluations and investigations.
-
Benefit Payments:
If the claim is approved, the provider begins paying benefits for medical expenses and lost wages. The frequency and amount of these payments will depend on the provider’s policies and state regulations.
-
Return to Work:
The provider often works with the employer and employee to facilitate a safe and timely return to work. This can include modified duty assignments or vocational rehabilitation.
-
Dispute Resolution:
If disputes arise regarding the claim, various dispute resolution methods are available, such as mediation or arbitration.
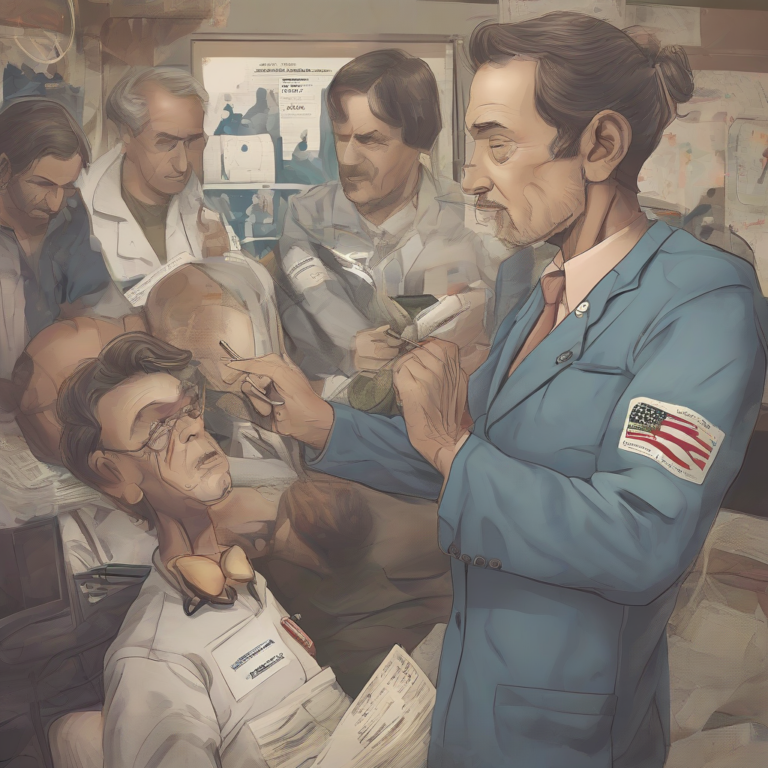
The Role of Healthcare Providers in Workers’ Compensation
Healthcare providers play a vital role in the workers’ compensation system. They provide medical treatment, assess the extent of injuries, and provide documentation for claims. Effective communication and coordination between healthcare providers and workers’ compensation providers are crucial for efficient claims processing and appropriate patient care.
-
Accurate Documentation:
Healthcare providers must meticulously document the patient’s injuries, treatment plan, progress, and prognosis. Accurate documentation is essential for supporting claims and ensuring timely benefit payments.
-
Compliance with Regulations:
Healthcare providers must adhere to all relevant state and federal regulations regarding workers’ compensation. This includes appropriate billing procedures and reporting requirements.
-
Communication with Providers:
Maintaining open communication with workers’ compensation providers helps streamline the claims process and ensures that patients receive appropriate care and benefits.
-
Independent Medical Examinations (IMEs):
In some cases, independent medical examinations are conducted to assess the extent of an employee’s injury and determine the need for ongoing treatment. These evaluations are often requested by the workers’ compensation provider.
Navigating Challenges in the Workers’ Compensation System
The workers’ compensation system, while designed to protect employees, can present challenges for both employers and employees. Understanding these challenges can help navigate the system more effectively.
-
Delayed or Denied Claims:
Claims can be delayed or denied due to various reasons, including disputes over the cause of injury, the extent of the injury, or the appropriateness of medical treatment. Understanding the grounds for denial and the appeals process is crucial.
-
Communication Barriers:
Effective communication between employers, employees, healthcare providers, and workers’ compensation providers is essential for a smooth claims process. However, communication breakdowns can lead to delays and frustration.
-
Navigating the Legal Aspects:
Workers’ compensation law can be complex, and navigating the legal aspects can be challenging. Seeking legal counsel if necessary can provide valuable support and guidance.
-
Return-to-Work Issues:
Facilitating a safe and timely return to work can be complex, especially for employees with significant injuries. Coordination between the employer, healthcare provider, and workers’ compensation provider is crucial for successful return-to-work outcomes.
-
Cost Containment:
Controlling the cost of workers’ compensation claims is a priority for both employers and insurers. This often involves strategies for injury prevention, early intervention, and efficient claims management.
Conclusion (Omitted as per instructions)